an email newsletter released every month highlighting the latest articles, events, technical inquiries, and voices from the community
COVID-19 Viral Mitigation and Decontamination
Posted on March 24, 2020 | Completed on March 24, 2020
For FDM printed parts that are replacing traditional parts which do NOT need to be sterilized (potentially: face shields, equipment housing etc.), what can be done to mitigate additional spread of the virus as those parts move through the fabrication, assembled and transported?
The Defense Systems Information Analysis Center (DSIAC) and the Homeland Defense & Security Information Analysis Center (HDIAC) were asked to provide quick answers to several questions to aid the COVID-19 response which largely revolve around the topics of decontamination and sterilization in advanced manufacturing of personal protective equipment (PPE). DSIAC and HDIAC contacted relevant subject matter experts with expertise in chemical, biological, radiological, nuclear, and explosive or advanced manufacturing and compiled their expert inputs into responses to each question posed. This response report addresses the risks of viral spread on parts fabricated through a large network of people and physical spaces; we provide recommendations of how to minimize these risks. We specifically address PPE printed using fused deposition modeling to describe methods that can be employed to mitigate additional spread of the virus during fabrication, assembly and transport. We highlight sterilization methods such as chemical methods (e.g., with bleach, alcohols, and hydrogen peroxide), heating and UV methods, ozone methods, and more. This report then briefly addresses methods of mitigating viral spread in solid part fabrication (e.g., laser-cut, computer numerical control, thermo-formed, vacuum-formed) specifically recommending UV use at a factory level, similar to what hospitals are doing, and possibly gas. This report then provides recommendations on specific chemicals, disinfectants, or processes that could be employed for a given list of material types: polymeric materials, polyactic acid, nylons, polyethylene terephthalate glycol, cellulose acetate, and Tyvek. We conclude with a list of recommended best practices to reduce viral loads and exposure risks to parts prior to later sterilization.
1.0 Introduction
To best answer the series of questions posed, DSIAC and HDIAC contacted relevant subject matter experts (SMEs) with expertise in chemical, biological, radiological, nuclear, and explosive or advanced manufacturing and compiled their responses. Additionally, we performed open-source and DTIC Research and Engineering (R&E) Gateway searches for relevant research and publications. The information included in this report is compiled from the expert opinions represented by DSIAC, HDIAC, America Makes, American Society of Mechanical Engineers (ASME), Stratasys, Texas Research Institute Austin (TRI-Austin), U.S. Army Test Evaluation Command (ATEC) Bio Test Division (CBC), U.S. Army ManTech, Naval Surface Warfare Center Dahlgren Division (NSWC-DD), Johns Hopkins University Applied Physics Laboratory (JHU APL), and others. Each of the questions is broken into its own section following the Introduction.
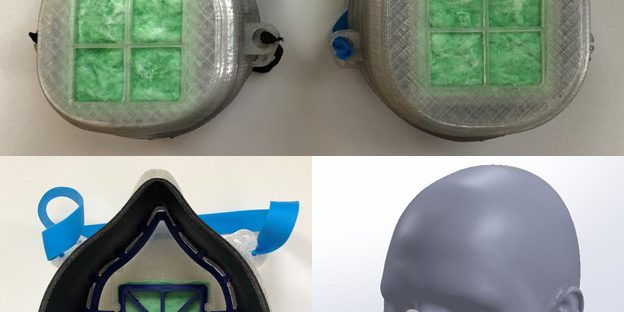
With the outbreak of COVID-19, a looming shortage of medical supplies required to treat the sick, and an additive manufacturing (AM) community eager to volunteer services, there is a need to coordinate and regulate three-dimensional (3-D) printed parts to produce, transport, and ultimately use in the healthcare community. America Makes and ASME are two additive manufacturing hubs for innovation, collaboration, and information dissemination that are striving to consolidate and simplify matching 3-D printing and healthcare communities.
America Makes is offering to assist in leading the effort to collect and distribute information relating to COVID-19 and AM, including collecting organizations/laboratories with the ability to use 3-D printing for parts and personal protective equipment (PPE) needed in the health care community [1]. America Makes is working with the Federal Drug Administration and National Institute to determine what PPE is needed, a means of centralized data collection, potential legal and IP issues, validation of models (being done currently at the U.S. Department of Veterans Affairs), and the evolving supply chain [2].
America Makes connected DSIAC with ASME’s Lauralyn McDaniel (McDanielL@asme.org, 212‑591-7024), who has 21 years of medical AM experience. She noted that FDM is typically not best suited for medical and/or sealing purposes due to the hard plastics (acrylonitrile butadiene styrene [ABS]/PLA) that serve as feedstocks. She added that stereolithography (SLA), digital light projector or selective laser sintering processes are better suited due to the flexibility of the resultant parts. Lauralyn was able to connect DSIAC with multiple AM experts and organizations that supplied input on the specific topics that follow [3].
Also offering their assistance during the global COVID-19 public health emergency is the American Society for Testing and Materials (ASTM) International. They are providing no-cost public access to important ASTM standards used in producing and testing PPEs—including face masks, medical gowns, gloves, and hand sanitizers—to support manufacturers, test labs, health care professionals, and the general public [4].
The overall consensus from the experts is that the AM community is eager to assist in any way possible, whether it be PPEs, critical medical parts, repairs, or even required tooling for other processes.
2.0 Is the cause for concern of increased viral spread on parts fabricated through a large network of people and physical spaces?
Steve Redifer (sredifer@hdiac.org), HDIAC Director and former commander of the Marine Corps Chem-Bio Incident Response Force, says the key is preventing infected people from entering the workspace and minimizing contact—as expected, the more people in the workspace, the better the chance for infection or contamination. He adds the following:
- Based on what is currently known about the novel coronavirus, it is spread from person‑to‑person and most frequently among close contacts (within about 6 ft). This type of transmission occurs via respiratory droplets.
- Transmission from surfaces contaminated with the virus has not been documented. There are some very preliminary studies on a few materials in the article “How Long Can the Novel Coronavirus Survive on Surfaces and in the Air?” [5]. Experts from TRI‑Austin note that there are still significant disagreements on the amount of time for various surfaces [6].
- Transmission of coronavirus occurs much more commonly through respiratory droplets than through fomites; however, current evidence suggests that novel coronavirus may remain viable for hours to days on surfaces made from a variety of materials.
- If there has been an infected person in the workspace, then there is a need to worry about the workspace being infected.
Mr. Redifer noted that if you are uncertain about contamination in the workplace, the whole place needs to be disinfected; cleaning of visibly dirty surfaces followed by disinfection is a best practice measure for prevention of COVID-19 and other viral respiratory illnesses in households and community settings. Once the facility is clean, then entry control is of primary concern.
COVID-19 can be killed by bleach/water, alcohol, and peroxide solutions. For disinfection, diluted household bleach solutions, alcohol solutions with at least 70% alcohol, and most common Environmental Protection Agency (EPA)-registered household disinfectants should be effective.
- Unexpired household bleach will be effective against coronaviruses when properly diluted.
- A bleach solution can be made by mixing the following:
- 5 tablespoons (1/3 cup) bleach per gallon of water or
- 4 teaspoons bleach per quart of water
After that, attention must be paid to people entering the facility. Everyone should have some sort of screening (for symptoms such as fever) prior to entry.
- For example, after initial screening, all employees should then enter a station where they wash their hands thoroughly 20 seconds or longer with friction—soap can break the envelope of the virus.
- If available, some sort of suit should be donned and rubber gloves worn; although wearing an N95 or N100 mask would be ideal, they are in short supply and reserved for healthcare professionals in most cases.
- Only after this is completed, should personnel be allowed to enter the facility.
Throughout operations, “social distancing (6 feet)” and regular hand washing must be enforced. As previously mentioned, the likelihood of infection/contamination goes up with a large number of people working in close quarters [7].
Doyle Motes (Non Destructive Evaluation Division Lead, dmotes@tri-austin.com, 512-263-2101 x293) and Richard Piner (rpiner@tri-austin.com) of TRI-Austin add that, in general, regardless of the method used, procedures would follow the same way the medical industry currently builds equipment. As long as parts are clean and dry when shipped, they should arrive at the assembly plant ready to use. If they are packed in a sealed container with drying agents, they should be free of virus at the other end (although a final disinfecting treatment may be recommended to make doubly sure of this due to the ambiguity associated with the virus’s survival time on free surfaces). Points of failure most likely to occur (but, unfortunately, not limited to because of “unknown, unknowns”) are (1) during transport (viral contamination of the exterior packaging surfaces) and (2) during unpacking/assembly and final use. There are several options available for cleaning the packaging if desired using chemicals, heat, light (ultraviolet [UV]), and ozone. Care must be taken to ensure that the choice of disinfection method for the particular article in question (i.e., cardboard packaging, blister packs, or the final component) will not damage the article and will be sufficient to remove any chance of viral transmission [6].
3.0 For FDM printed parts replacing traditional parts that do NOT need sterilized (potentially, face shields, equipment housing, etc.), what can be done to mitigate additional spread of the virus as those parts move through fabrication and assembled and transported?
There are three keys steps in the AM process that would be of concern for the spread of a viral load: (1) fabrication (printing), (2) post-processing (support removal, assembly, and cleaning), and (3) packaging/delivery.
Adam Pawloski (Vice President of Manufacturing Solutions, adam.pawloski@stratasys.com), Chaffee Tran (Director of Materials Product Management, chaffee.tran@stratasys.com), and Evan Hochstein (Healthcare Solutions Engineer, evan.hochstein@stratasys.com) of Stratasys, an FDM machine manufacturer, and TRI-Austin note that the FDM process inherently should kill any biological agent that might be on the surface of the raw feedstock due to the high temperatures required to melt the plastic, whether ABS, PLA, etc. [6, 8].
Specifically, starting at fabrication, the high temperatures associated with FDM process as the material is melted for printing (usually in excess of 150 °C [302 °F] for most FDM materials) will kill any virus on the material as it is being printed onto the build plate of an FDM printer. In addition, the build plate must be heated to between 50 and 100 °C to ensure that the part being printed appropriately adheres to the build plate. However, once humans start handling the part, the potential for the virus to spread exists. One example is removing components from the build plate of an FDM printer, as this can require “persuasion” to remove the component from the build plate intact and necessitate handling of the component, build plate, 3-D printer, and tooling to remove the component. Therefore, using proper precautions (masks, gloves, and clean environment) and clean tools is extremely important [6, 8].
It is recommended that immediately after building, the part be disinfected via a means that considers the material makeup of the component to not damage it (see the following sections for recommendations), as certain FDM materials react differently to various cleaning agents [6, 8]. Mr. Pawloski recommended submerging finished parts in a bath of isopropyl alcohol as the best way to clean parts, as the material would not have any adverse reactions, the alcohol could penetrate the inherent porosity, and it would quickly dry as the alcohol is volatile. For example, some agents can cause stress cracking or melting (as for ABS plastic and acetone) [8]. The part should then be sealed in plastic with a desiccate pack (if available) to remove any water from the part that the virus could survive on.
As many of the FDM components may be provided by nontraditional manufacturers (e.g., a 3-D printer hobbyist printing PLA ventilator valves in his garage and donating them), the cleanliness of the packaging and components cannot be assured upon arrival at the next point of delivery in the supply chain (either storage or final point of use). For this reason, a final treatment at the point of use is recommended. Along this line, options for bulk cleaning include chemical dips, ozone treatments, heating, and UV exposure [6].
3.1 Chemical Methods
There are three simple chemical solutions effective for cleaning—bleach (sodium hypochlorite), alcohols, and hydrogen peroxide.
3.1.1 Bleach (Sodium Hypochlorite)
If you use bleach, use 1/4 cup of bleach per 1 gallon of cold water, but be sure to follow directions on the product label. Make the diluted bleach solution as needed and use within 24 hours, as its disinfecting power fades with time [6]. Mr. Pawloski warns against using bleach on any FDM part except the most chemically-resistant plastic because most feedstocks won’t “behave” and will weaken [8].
2.3.1.2 Alcohols
Many forms of alcohol, including rubbing alcohol, can kill germs. Diluted alcohol can be mixed with water (or aloe vera) to make hand sanitizer, but the alcohol concentration should be between 60% and 70% to kill coronaviruses. This is already a common way to clean FDM parts in post-processing, especially in a bath to remove loose, internal supports [6, 8].
2.3.1.3 Hydrogen Peroxide
Hydrogen peroxide is typically sold in concentrations of about 3%. It can be used as is or diluted to 0.5% concentration for effective use against coronaviruses on surfaces. It should be left on surfaces for 1 minute before wiping.
All chemicals used have a “contact time” that is required to ensure viral destruction. These times are typically 3 to 10 minutes. This method can be scaled up for a point-of-use final decontamination via a chemical dip operation [9, 10].
In addition to these, other viral killers are listed in subsequent sections of this report, as well as material responses to these and other chemicals.
3.2 Heating and UV Methods
There is little lab work reported on deactivating the specific virus causing the pandemic (COVID-19), as it is new and there has not been enough time to perform experiments. However, most experts believe that severe acute respiratory syndrome (SARS)-CoV-2 is very similar to the virus that caused the SARS outbreak of the early 2000s. From previous experiments on SARS, viruses remained stable at 4 °C (39.2 °F), at room temperature (20 °C or 68 °F), and at 37 °C (98.6 °F) for at least 2 hours without remarkable change in the infectious ability in cells; however, these viruses were converted to be noninfectious after 90-, 60-, and 30-minute exposures at 56 °C (132 °F), 67 °C (153 °F), and 75 °C (167 °F), respectively. Irradiation via UV for 60 minutes on the virus in culture medium resulted in the destruction of viral infectivity down to the undetectable level. The survival ability of SARS coronavirus in human specimens and in environments seems to be relatively strong. Heating and UV irradiation can efficiently eliminate the viral infectivity. We also note that the previous works used UV-A radiation (315–400 nm). UV-C (100─280 nm), which is a higher energy and naturally filtered from the ground by Earth’s atmosphere, should render a surface free of active virus in 15 minutes or less. TRI-Austin notes that appropriate precautions must be taken if utilizing UV radiation to prevent injury [6]. Stratasys warns against steam sterilization with FDM parts. Stratasys and Dr. Jennifer Therkorn of JHU APL warn that UV treatments may not be as effective on FDM parts due to the inherent part porosity that a surface-based treatment would not properly decontaminate [8, 11].
In addition, UV irradiation may be effective to disinfect working shops and laboratories these components are being made in, provided that safety precautions are followed. More research is needed on this topic to provide educated recommendations [6].
3.3 Ozone Methods
The use of short-wave UV (especially UV-C) light in air will also produce ozone due to the presence of atmospheric oxygen. Ozone will attack both bacteria and viruses. However, it should be noted that to reach 100% destruction in less than an hour, ozone levels need to be more the 0.6 ppm. More than 0.1 ppm is considered harmful to human health. So, to use ozone to clean a surface, it would need to be done in a sealed chamber. In addition, materials should be considered, which are described in the last section [6].
3.4 Further Input
For further input, DSIAC reached out to Dr. Bryan Tienes (bryan.tienes@navy.mil, 301-744-5564) of the Chemical Biological Radiological (CBR) Defense Division of the NSWC Indian Head Explosive Ordnance Disposal Technology Division for support [12]. He was able to assist in getting the input of researchers from NSWC-DD and JHU APL.
3.5 Decontaminating AM Parts
Dr. Jennifer Therkorn (Jennifer.Therkorn@jhuapl.edu, 240-228-4707) is an applied biological sciences senior scientist at JHU APL. She collected the following information [11]:
- 3-D printed parts can have a porosity to them due to incomplete fusing of deposited layers; this would require a soaking or “vapor” approach to get within all crevices.
- First steps should include cleaning with detergent solutions/soap if possible. Dr. Therkorn said, “I’ve shown in past work that a 10-minute ultrasonication can greatly help to remove microbes from 3-D print materials, which would be good to do in a soapy solution” [13].
- Soaking in diluted household bleach or >70% alcohol solutions should be effective with sufficient contact time (at least 20 minutes). “I have seen evidence showing bleach does not destroy PLA, but I can’t speak for other materials on the list,” Dr. Therkorn added.
- If soaking is not preferred, other approaches might include vaporized hydrogen peroxide. This method has been shown to possibly have good efficacy against enveloped viruses [14].
- If only a surface decontaminant is required, then methods such as UV exposure and surface wipe cleaning with EPA-approved cleaning agents may also be tested. However, repeated exposure of plastics to UV can cause degradation.
Dr. Tienes called Dr. Tony Buhr (tony.buhr@navy.mil, 540-653-0061), NSWC’s expert and one of the nation’s top experts in biological warfare agent decontamination. Dr. Buhr is a principal scientist in the CBR Concepts and Experimentation Branch at NSWC-DD. He recently submitted a paper for publication in which he extrapolated and collected on decontamination rates of hot humid air on an appropriate biological surrogate to enveloped viruses such as COVID-19. His input is as follows [15]:
- Dahlgren Decon will kill spores, vegetative cells, and nonenveloped virus, all of which are considered more difficult to kill than nonenveloped, virus-like coronavirus. Spores are considered the most difficult biological cells to kill, so the attachments are focused on spore inactivation. PES Solid is the critical ingredient. We did not test enveloped virus such as corona in the attachments since enveloped virus is considered easier to kill than the tested organisms.
- Hot, humid air also works on materials. Hot, humid air has limited applications because environmental chambers are needed. It may be a consideration for high-value materials with limited materials compatibility.
- We would consider surfactants, detergents, and soaps as critical ingredient(s) to disinfect enveloped virus, as the envelope membrane of the virus should be susceptible to being dissolved. Current speculation is that the virus may be protected by mucin after it is coughed up. Surfactants, detergents, and soap solutions will also be needed to cover surfaces and to disassemble any protective mucin/host cell debris that accompanies the virus. Soapy solutions with common reactive ingredients, including bleach, pH-adjusted bleach, peracids (PES Solid), and hydrogen peroxide, should kill the virus.
- With respect to PES Solid, there is a limited supply, as it is made by Solvay in Germany. There may be alternative safer methods to manufacture PES Solid but that would take some research. In 2019, we tested PES Solid at 10x lower concentration than what was published in 2013–2014—it still killed spores.
3.6 Prevention of Virus Spread Throughout the Supply Chain
Recommended cleaning procedures (as recommended by the Centers for Disease Control [CDC]) are as follows:
- Wear disposable gloves when cleaning and disinfecting surfaces. Gloves should be discarded after each cleaning. If reusable gloves are used, those gloves should be dedicated for cleaning and disinfection of surfaces for COVID-19 and should not be used for other purposes. Consult the manufacturer’s instructions for cleaning and disinfection products used. Clean hands immediately after gloves are removed.
- If surfaces are dirty, they should be cleaned using a detergent or soap and water prior to disinfection.
- For disinfection, diluted household bleach solutions, alcohol solutions with at least 70% alcohol, and most common EPA-registered household disinfectants should be effective.
- Diluted household bleach solutions can be used, if appropriate, for the surface. Follow manufacturer’s instructions for application and proper ventilation. Check to ensure the product is not past its expiration date. Never mix household bleach with ammonia or any other cleanser. Unexpired household bleach will be effective against coronaviruses when properly diluted. Prepare a bleach solution by mixing:
- 5 tablespoons (1/3 cup) bleach per gallon of water or
- 4 teaspoons bleach per quart of water
- Products with EPA-approved emerging viral pathogens claims are expected to be effective against COVID-19 based on data for harder-to-kill viruses. Follow the manufacturer’s instructions for all cleaning and disinfection products (e.g., concentration, application method and contact time, etc.).
- Diluted household bleach solutions can be used, if appropriate, for the surface. Follow manufacturer’s instructions for application and proper ventilation. Check to ensure the product is not past its expiration date. Never mix household bleach with ammonia or any other cleanser. Unexpired household bleach will be effective against coronaviruses when properly diluted. Prepare a bleach solution by mixing:
- For soft (porous) surfaces such as carpeted floor, rugs, and drapes, remove visible contamination if present and clean with appropriate cleaners indicated for use on these surfaces. After cleaning:
- Launder items, as appropriate, in accordance with the manufacturer’s instructions. If possible, launder items using the warmest appropriate water setting for the items and dry items completely.
- Use products with the EPA-approved emerging viral pathogens that are suitable for porous surfaces.
If heating is used, then the temperature must be as high as possible without damaging any components or packaging (as broad knowledge of the packaging material’s thermal properties should be known to ensure this).
3.7 Clothing, Towels, Linens and Other Items That Go in the Laundry
Wear disposable gloves when handling dirty laundry from an ill person and then discard after each use. If using reusable gloves, those gloves should be dedicated for cleaning and disinfecting surfaces for COVID-19 and should not be used for other household purposes. Clean hands immediately after gloves are removed [6].
- If no gloves are used when handling dirty laundry, be sure to wash hands afterwards.
- If possible, do not shake dirty laundry. This will minimize the possibility of dispersing the virus through the air.
- Launder items, as appropriate, in accordance with the manufacturer’s instructions. If possible, launder items using the warmest appropriate water setting for the items and dry items completely. Dirty laundry from an ill person can be washed with other people’s items.
- Clean and disinfect clothes hampers according to previous guidance for surfaces. If possible, consider placing a bag liner that is either disposable (can be thrown away) or can be laundered.
The components should be disinfected after fabrication, placed in packaging, and shipped. Upon reaching a destination, it is recommended that all precautions be taken as though the packaging is contaminated (use of disposable gloves, hand washing, etc.). It is recommended that this be done for every destination unless a trusted supply chain can be established (and depending on the circumstances, it may need to be continued after that). As discussed, it is also recommended that final disinfecting (based on what is available and the limitations associated with the material properties) be conducted when the material is unpackaged and assembled for use [6, 7].
For more information, please refer to the following:
- Duan, S., X. Zhao, R. Wen, and J. Huang. “Stability of SARS Coronavirus in Human Specimens and Environment and Its Sensitivity to Heating and UV Irradiation.” Biomedical and Environmental Sciences, vol. 16, issue 3, pp. 246–255, 2003.
- Welch, D., M. Buonanno, V. Grilj, I. Shuryak, C. Crickmore, A. Bigelow, G. Randers-Pehrson, G. W. Johnson, and D. J. Brenner. “Far-UVC Light: A New Tool to Control the Spread of Airborne Mediated Microbial Diseases.” Scientific Reports, vol. 8, article 2752, 2018.
- Henwood, F. “Coronavirus Disinfection in Histopathology.” Journal of Histotechnology, pre-print available, 2020.
4.0 For solid parts (laser-cut, CNC, thermo-formed, vacuum-formed) that are replacing traditional parts which are NOT sterilized, what can be done to mitigate virus spread?
As far as any processes Army ManTech has worked on or is working on related to sterilization/decontamination of an entire manufacturing process (fabrication, assembly, packaging/shipping), there are none. Their suggested approach to decontamination at the facility level was UV use, similar to what hospitals are doing, and possibly gas. However, Army ManTech is having difficulty in finding manufacturers of the UV equipment that could provide supply, especially non-China sources. Use of any other spectrum of radiation (i.e., X-ray) for decontamination were not viewed favorably for implementation [16]. DSIAC requested assistance through the U.S. Army Combat Capabilities Development Command (CCDC) Director for Enterprise Programs at the Plans, Programs, and Assessments (G5) Office (Program Manager for Army ManTech) in providing a designated SME point-of-contact for the panel and obtaining a copy of CCDC’s internally solicited information on ideas to help address the COVID-19 crisis.
TRI-Austin notes that for most of these materials, the same processes and treatment agents would be the same as in Section 2.3. However, metallic materials are, in general, more resistant to chemical attack than polymers. Their main disadvantage in the present crisis is that specialized equipment and training is required to produce parts. In addition, the time required and amount of money per part are significantly less than what can be achieved through FDM
3-D printing [6].
5.0 Can someone recommend specific chemicals, disinfectants, or processes (soap/water washing) that could be employed for the following materials: PLA, PETG, Acetate, nylon family, tyvek, and nonpermeable textiles?
DSIAC searched open sources and the DTIC R&E Gateway for relevant literature and determined that there is no specific literature available that provides recommendations on specific chemicals, disinfectants, or processes for the listed materials. The most relevant source identified was the “List N” document [17], independently recommended by SMEs from CCDC CBC [18].
According to the EPA [17]:
“While these products have not been tested against SARS-CoV-2, the cause of COVID-19, they are expected to be effective based on demonstrated efficacy against a harder‑to‑kill virus, qualified for the emerging viral pathogens claim, and/or demonstrated efficacy against another human coronavirus similar to SARS-CoV-2.”
The EPA is continuing to update the list as new information is becoming available.
With respect to the pervious questions, we will discuss the effects associated with plastic materials. In addition, regarding “any other non-permeable textiles,” this category is quite broad, meaning the potential materials and their respective properties are such that they will need to be addressed on a case-by-case basis.
A CCDC CBC decontaminant SME provided the following comments and recommendations [18]:
Broadly speaking, the disinfectant falls in four categories:
- Chlorine-based
- Peroxide-based
- Quaternary ammonium compound (quat) salts
- Some sort of alcohol/IPA (60%─70%).
They all have their pros and cons.
- If surface corrosion is not an issue, chlorine-based products are recommended (0.1%–1%), with a minimum of 10–20 minutes of contact time. These are also cheap.
- It requires a post-rinsing step to remove the chlorine residues.
- If cost is not an issue, Peridox (ready-to-use) and/or other per-acetic acid/peroxide-based products are highly effective and may not require post-decontaminant rinsing because the ingredients degrade to water and oxygen.
- Alcohol-based products are also effective but require a minimum of 20–30 minutes of contact time and are less effective if the virus is mixed with other body fluids. They are also flammable and may require specific storage conditions.
- Quats will be my last choice because they leave residues and are less effective than the other three classes.
- For the type of material (fabric), I would pick chlorine-based products (0.5%).
5.1 Polymeric Materials
Polymers, especially 3-D printed ones, offer the advantage of significantly faster turnaround time to the end user. That said, there are several items that must be understood here. There is a lack of consistent data available for thermoplastics capable of being quickly and easily 3-D printed. We have compiled datasets available from online searches, but these are often contradictory, with similar potential chemical compounds yielding wildly different results (for this, the DSIAC-compiled list from Dr. Brian Bennet was used that identified products with emerging viral pathogens and human coronavirus claims for use against SARS-CoV-2, with the addition of UV light and ozone disinfecting).
For the thermoplastics mentioned (Tyvek [essentially, high-density polyethylene], the nylon family, PETG, PLA, and cellulose acetate), there are a number of additives (such as dyes to change colors like titanium dioxide [TiO2]), which is used to color plastics white) that cause a change in behavior in the material’s glass transition or softening temperature (when the material can no longer hold its shape) and the material’s reaction to different chemicals/processes used as disinfecting agents.
In addition, molecular weight of the individual polymer chains within the plastic causes a great deal of differences in material behavior (high molecular weights lead to greater crystallinity, greater softening temperatures, and better chemical resistance). All these factors are determined by the manufacturer of the feedstock material used to fabricate a plastic part (either by injection molding or 3-D printing).
Unfortunately, when filament is sold for printing, it is not packaged or marked in such a way that reveals the specifics of the feedstock, rather it is sold as only PLA, nylon, PETG, etc. Sometimes, the seller will have material batch information that can be used to trace the chemistry of the material, but this is often not the case. As a result, material behavior is not necessarily predictable from vendor to vendor.
In addition, much of the published material on chemical resistance is taken at different temperatures, meaning there can be discrepancies, such as a common chemical damaging a material under hot conditions, but none under cold conditions. Testing temperatures on published materials are not always stated.
5.2 Polylactic Acid (PLA)
By far, the most commonly available plastic material for 3-D printing, PLA, is capable of being turned into components by individuals ranging from garage hobbyists to professionals. It is biodegradable (over 6–24 months), meaning any plastic parts could be recycled into the ground. Data on the chemical resistance of PLA to many of the chemicals of choice here is not readily available. Ethanol and isopropyl alcohol have been proven to not damage the material for disinfecting, and sodium carbonate-based cleaners may be appropriate for use.
High heat (in excess of 55 °C or 131 °F) is not recommended, as this is past the softening temperature (many hobbyists have complained about PLA softening or losing its shape when left in a hot car), unless the vendor specifically designates the material as a high-temperature PLA (now available) capable of retaining structural features at temperatures as high as ~90 °C (194 °F). UV light will damage PLA (decreasing the molecular weight of the individual molecules), resulting in loss of structural properties and chemical resistance. It is recommended that UV disinfecting treatments only last the minimum time needed to kill the viruses on the surface and no longer. Ozone treatments are recommended to last no more than 10 minutes to preserve material properties (based on the best, currently-available data). This UV exposure time can be increased, but the reusability of the component may be compromised.
Soap and water can be used for washing, but the PLA component should be removed when the process is finished and not allowed to sit in the water for long periods to avoid material swelling and premature decomposition starting.
5.3 Nylons
Nylon is another very popular 3-D printed material and the one with the most data available regarding chemical resistance, owing to its use around hazardous materials in the chemical processing and oil and gas industries. There are a very large number of variations on nylon—the data varies considerably, depending on the composition of the material in question.
Universally accepted is that phenol-based cleaners will dissolve nylon and are to be avoided. Hydrogen peroxide, sodium hypochlorite (common bleach), citric acid, triethylene glycol, and potentially isopropyl alcohol (this compound is stated in some cases to be acceptable and others to be avoided) are not recommended (based on currently-available data). Ammonium based, sodium carbonate-based ethanol, and L-lactic acid are believed to be acceptable (based on currently-available data).
UV will cause nylon to degrade (depending on the strength of the light, its wavelength, and nylon-specific material). Washing in soap and water is acceptable, but water will cause the nylon to swell some (uptake water) and lose dimensional tolerances to some extent. The softening temperature can be as low as 55 °C (131 °F). No data are available on using ozone as a disinfectant.
5.4 Polyethylene Terephthalate Glycol (PETG)
PETG is a less popular material for 3-D printing but is very popular for use in food storage containers (it is the material disposable water bottles are made from). Unfortunately, little information is available on its chemical resistance. Areas that are recommended to avoid are ammoniums, phenols, sodium hypochlorite (bleach), and sodium carbonate-based cleaning solutions.
Ethanol is believed to be acceptable, with conflicting information about isopropyl alcohol. Soap and water are acceptable for washing. PETG will accept heating to a higher temperature (~80 °C or 176 °F). Anecdotal information claims that its UV resistance is better than the other plastics listed here. No currently available data are available on its resistance to ozone [6].
5.5 Cellulose Acetate
Cellulose acetate is another less commonly used 3-D printing material. Again, little information is available its chemical resistances. Phenols are to be avoided, as the material may dissolve when washed in water. Potentially acceptable are using hydrogen peroxide, ethanol, isopropyl alcohol, and ammonium-based cleaners. Cellulose acetate has a higher softening temperature of ~100 °C (212 °F), but no data are available regarding the effects of ozone. The material does degrade in the presence of UV light, but adding TiO2 can mitigate these effects.
5.6 Tyvek
Tyvek is the trade name for the high molecular weight polyethylene from DuPont used to make industrial protective equipment, such as hazmat suits. In general, Tyvek is chemically resistant to a wide variety of materials over the short term. It is partially resistant to UV radiation and ozone and has a softening temperature of 110 °C (230 °F).
A list of the effects of the cleaning agents provided by the CBC from Dr. Brian Bennett is delineated in Table 1. We strongly note that these are open-literature sources from a number of different manufacturers (listed after the table) performing tests in different ways on potentially-different material systems with significant holes in the data. This list is only a guide and should not be used as a final answer to the problem but rather to direct next steps [6].
Table 1: List of Known Viral Killers and Their Effects on Polymers of Interest.csv
| Viral Killers | Tyvek | Nylon(s) | PLA | PETG | Cellulose Acetate |
|---|---|---|---|---|---|
| Quaternary Ammonium | possibly acceptable | believed to be acceptable | no data available at this time | potential dissolution | possibly acceptable |
| Hydrogen Peroxide | believed to be acceptable | not recommended | no data available at this time | no data available at this time | possibly acceptable |
| Phenol-Based Solutions | not recommended | not recommended | no data available at this time | not recommended | not recommended |
| Ethanol | believed to be acceptable | acceptable | acceptable | believed to be acceptable | believed to be acceptable |
| Isopropanol (Same as Isopropyl Alcohol) | believed to be acceptable | disagreement in literature | acceptable | disagreement in literature | believed to be acceptable |
| Peroxyacetic (Peracetic) Acid | no data available at this time | no data available at this time | no data available at this time | no data available at this time | no data available at this time |
| Sodium Hypochlorite | believed to be acceptable | not recommended | no data available at this time | not recommended | no data available at this time |
| Dischloroisocy-Anurante Dihydrate | no data available at this time | no data available at this time | no data available at this time | no data available at this time | no data available at this time |
| Silver Ions/Citric Acid | believed to be acceptable | not recommended | no data available at this time | not recommended | disagreement in literature |
| Hypochlorous Acid (HOCl) | no data available at this time | no data available at this time | no data available at this time | no data available at this time | no data available at this time |
| Octanoic Acid | no data available at this time | no data available at this time | no data available at this time | no data available at this time | no data available at this time |
| Sodium Carbonate | no data available at this time | acceptable | possibly acceptable | not recommended | no data available at this time |
| Triethylene Glycol | no data available at this time | not recommended | no data available at this time | no data available at this time | no data available at this time |
| L-Lactic Acid | believed to be acceptable | not recommended | no data available at this time | no data available at this time | no data available at this time |
| Glycolic Acid | no data available at this time | no data available at this time | no data available at this time | no data available at this time | no data available at this time |
| Ammonium Carbonate | possibly acceptable | believed to be acceptable | no data available at this time | no data available at this time | possibly acceptable |
| Ammonium Bicarbonate | possibly acceptable | believed to be acceptable | no data available at this time | no data available at this time | possibly acceptable |
| UV Radiation | slight degradation over time from constant/ repeated exposure | degradation over time from constant/ repeated exposure | significant degradation over short term | degradation over time from constant/ repeated exposure | degradation over time from constant/ repeated exposure |
| Soap and Water | acceptable | acceptable (will swell) | acceptable | acceptable | not recommended |
| Glass Transition (Softening) Temperature | 110 °C (230 °F) | 55 °C (131 °F) | 55 °C (131 °F), other versions can reach 110 °C (230 °F) | 80 °C (176 °F) | 100 °C (212 °F) |
| Ozone | partially resistant | no data available at this time | no more than 10 minutes per exposure | no data available at this time | no data available at this time |
Table 1 Source Links:
- https://www.calpaclab.com/chemical-compatibility-charts/
- https://kuhnke.kendrion.com/attachment/ICS/ics_pdf_brochure/ics_pdf_chemical-resistance-2015_en.pdf
- https://omnexus.specialchem.com/polymer-properties/properties/glass-transition-temperature
- http://www.sdplastics.com/kingplastic/Chemical-Resistants-Chart.pdf
- http://kmac-plastics.net/data/chemical/petg-chemical.htm#.Xnlxnkp7lPY
- http://tools.thermofisher.com/content/sfs/brochures/D20480.pdf
- https://www.toray.jp/plastics/en/amilan/technical/tec_004.html
- https://www.newmantools.com/pipestoppers/NYLON_chem_resistance_nt.pdf
- https://www.curbellplastics.com/Research-Solutions/Technical-Resources/Technical-Resources/Chemical-Resistance-Chart
- https://www.usplastic.com/catalog/files/charts/LG%20CC.pdf
- https://www.eastman.com/Literature_Center/P/PP101.pdf
Table 1 References:
- Puls, J., S. Wilson, and D. Holter. “Degradation of Cellulose Acetate Based Materials: A Review.” Journal of Polymers and the Environment, vol. 19, pp. 152–165, 2011.
- Zhang, C., S. Rathi, J. Goddard, K. Constantine, and P. Collins. “The Effect of UV Treatment on the Degradation of Compostable Polylactic Acid.” Journal of Emerging Investigators, November 2013.
- Eren, H. A., O. Avinc, P. Uysal, and M. Wilding. “The Effects of Ozone Treatment on Polylactic Acid (PLA) Fibres.” Textile Research Journal, March 2011.
- Sato, S., D. Gondo, T. Wada, S. Kanehashi, and K. Nagai. “Effects of Various Liquid Organic Solvents on Solvent-Induced Crystallization of Amorphous Poly(lactic acid) Film.” Journal of Applied Polymer Science, pp. 1607–1617, 2013.
6.0 For parts that will ultimately be sterilized, what are best practices to reduce viral loads and exposure risks prior to being sterilized?
William Davis, a SME with ATEC CBC on Dugway Proving Ground, UT, notes that the best practice for minimizing contamination before sterilization is a cover of some kind. This is not always easy or practical in a manufacturing environment. Some of the literature seem to indicate that without touching the skin to the surface, there would be minimal spread to individuals. Rigorous enforcement of fresh, clean gloves will minimize touching of contaminated surfaces with subsequent transfer to the skin. To mitigate spread, sterilization and then covering will minimize recontamination and spread of the virus [19].
The basic question here is how the chosen decontamination solutions will interact with these materials; this will be manufacturer and material specific.
The CDC recommends alcohol and/or bleach/water solutions for decontamination—hence, the question will be material-specific based on the selected decontamination substance (e.g., bleach/water and alcohol).
It can be noted that bleach/water is a standard decontamination agent for biological agents, and decontamination is regularly performed in Tyvek suits and other nonpermeable textiles. Note that Tyvek is a brand name, and the breakthrough time will vary based on the product—these breakthrough times are available through the manufacturer [7].
References
[1] America Makes. “COVID-19 Needs and Capabilities Repository.” https://www. americamakes.us/statement-on-covid-19/, accessed 24 March 2020.
[2] Martof, A., B. Ribic, A. Resnick, and J. Wilcynski. America Makes. Personal communication, 23 March 2020.
[3] McDaniel, L. ASME. Personal communication, 24 March 2020.
[4] ASTM International. “ASTM Standards & COVID-19.” https://www.astm.org/COVID-19/, accessed 25 March 2020.
[5] The Economist. “How Long Can the Novel Coronavirus Survive on Surfaces and in the Air?” https://www.economist.com/graphic-detail/2020/03/19/how-long-can-the-novel-coronavirus-survive-on-surfaces-and-in-the-air?utm_campaign=the-economist-today&utm_medium=newsletter&utm_source=salesforce-marketing-cloud&utm_term=2020-03-19&utm_content=article-link-4, 19 March 2020.
[6] Motes, D., and R. Piner. TRI-Austin. Personal communication, 24 March 2020.
[7] Redifer, S. HDIAC. Personal communication, 23 March 2020.
[8] Pawloski, A., C. Tran, and E. Hochstein. Stratasys. Personal communication, 24 March 2020.
[9] Preidt, R. “The Most Effective Ways to Kill Coronavirus in Your Home.” WebMD. https:// www.webmd.com/lung/news/20200318/the-most-effective-ways-to-kill-coronavirus-in-your-home#1, 18 March 2020.
[10] CDC. “Clean & Disinfect.” https://www.cdc.gov/coronavirus/2019-ncov/prepare/cleaning-disinfection.html, accessed 23 March 2020.
[11] Therkorn, J. Johns Hopkins University Applied Physics Laboratory. Personal communication, 24 March 2020.
[12] Tienes, B. M. NSWC Indian Head EOD Technology Division, CBR Defense Division. Personal communication, 23 March 2020.
[13] Therkorn, J., N. Thomas, L. Calderon, J. Scheinbeim, and G. Mainelis. “Design and Development of a Passive Bioaerosol Sampler Using Polarized Ferroelectric Polymer Film.” Journal of Aerosol Science, vol. 105, pp. 128–144, March 2017, https://www. sciencedirect.com/science/article/pii/S0021850216301707#f0025, 21 December 2016.
[14] Goyal, S.M., Y. Chandler, S. Yezli, and J. A. Otter. “Evaluating the Virucidal Efficacy of Hydrogen Peroxide Vapour.” J Hosp Infect, vol. 86, no. 4, pp. 255–259, April 2014, https://www.ncbi.nlm.nih.gov/pubmed/24656442, 27 February 2014.
[15] Buhr, T. Naval Surface Warfare Center Dahlgren Division. Personal communication, 23 March 2020.
[16] U.S. Army ManTech. Personal communication, 23 March 2020.
[17] Environmental Protection Agency. “List N: Disinfectants for Use Against SARS-CoV-2.” https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2, updated 19 March 2020.
[18] Deputy Director. U.S. Army CCDC CBC. Personal communication, 25 March 2020.
[19] Davis, W. U.S. Army Test Evaluation Command Bio Test Division. Personal communication, 23 March 2020.
Want to find out more about this topic?
Request a FREE Technical Inquiry!

